GYN Atlas - Low-Grade Squamous Intraepithelial Lesion
SQUAMOUS CELLS
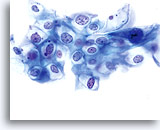
LOW-GRADE SQUAMOUS INTRAEPITHELIAL LESION (LSIL)
Diane D. Davey, MD
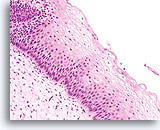
Squamous dysplasia is characterized by the presence of at least some squamous features in the cytoplasm of the abnormal cells. (Suggested Reading 1) The grade of dysplasia mirrors the maturity of the cells involved. For example, cells of mild dysplasia resemble mature metaplastic, superficial and intermediate cells while more severely dysplastic epithelium reflects less mature normal epithelium such as parabasal and/or immature metaplastic type cells. With the emergence of “The Bethesda System for Classification of Cervical Vaginal Diagnoses” the use of the term “dysplasia” lessened in favor of low-grade squamous intraepithelial lesions (LSIL) or high-grade squamous intraepithelial lesions (HSIL). We will use the Bethesda System (2014) terminology throughout this atlas.
The morphology of LSIL (including human papillomavirus (HPV)-associated changes) on the ThinPrep slide is essentially identical to LSIL on the conventional Pap. In part, this similarity is due to the ability of the mature squamous cell to maintain its integrity in spite of inadequate fixation or smear artifact inherent with the conventional smear. This integrity is a result of cell rigidity due to cytoplasmic keratinization.
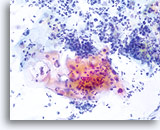
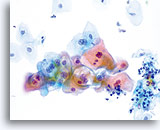
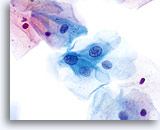
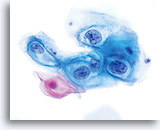
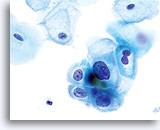
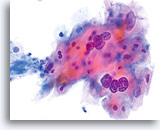
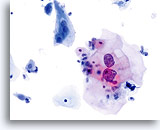
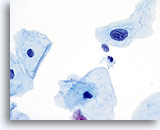
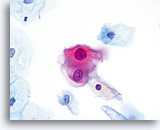
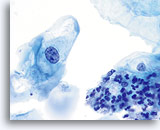
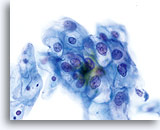
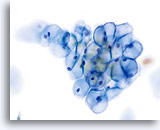
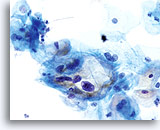
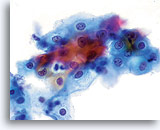
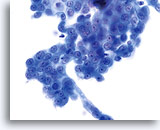
Because of their morphology, cells derived from low-grade lesions are among the most easily located and recognized of intraepithelial abnormalities. Comparatively, LSIL nuclei are the largest and exhibit a lower N/C ratio than HSIL or carcinoma. These cells have greater nuclear atypia than ASCUS, exhibited as increased nuclear size, chromatin irregularity and irregularity of the nuclear envelope. Nuclei may occasionally not be as hyperchromatic as on conventional smears, but they are always hyperchromatic compared to the surrounding normal cells. The HPV-associated changes (e.g. cavitation of the cytoplasm) are more prominent due to the wet fixation as well as the transfer technique, which eliminates cell distortion caused by the conventional smearing method. The ThinPrep method better preserves these cell changes allowing for easier differentiation between true HPV-induced cytoplasmic cavitations and benign/degenerative vacuoles and/or glycogenated squamous cells.
Because the cells are mature squamous cells, they retain their polygonal shape and for the most part retain their normal size. The nuclei are enlarged at least 3-4 times that of the normal intermediate cell nucleus, however, when HPV changes are evident, the cells may be smaller (almost parakeratotic) and the nuclei may also be smaller and somewhat pyknotic appearing with binucleation and/or multinucleation present. These pyknotic nuclei will also exhibit abnormal features such as hyperchromasia, increased size from that of the normal superficial squamous cell and a slight variation in shape and size. It is important to stress that an interpretation of LSIL/HPV requires both clear-cut cytoplasmic cavitations accompanied by the abnormal nuclear morphology described above.
Some SIL cases exhibit a mixture of LSIL and HSIL cells, and the most severe abnormality should take precedence when interpreting the ThinPrep. Occasionally it is difficult to distinguish LSIL from HSIL. Features favoring HSIL include a high N/C ratio, immature cytoplasm, and greater nuclear abnormalities. Rare SIL cases cannot be categorized either due to paucity of abnormal cells or truly intermediate criteria. Such cases may be more likely to progress, and an interpretation of “SIL, grade cannot be determined” or similar terminology is most prudent. While biopsy follow-up studies of LSIL will most frequently show low grade biopsy changes, about 15-20% of LSIL cases are followed by high grade biopsies.
LOOK-ALIKE ENTITES (Differential Diagnoses):
True to form, LSIL has a few key look-alike entities, although they are somewhat easier to differentiate because of the immediate fixation with the ThinPrep® Pap Test resulting in better visualization of the cells and their features. For the differential criteria and images of LSIL to ASCUS, refer to the ASCUS chapter.
| REACTIVE (organism or inflammation) |
Repair (typical) |
LSIL (HPV) |
|
| Cellular Presentation | Single or in sheets | Flat sheets and groups | Single or in sheets |
| Cell Type | All cell types affected | Endocervical/ metaplastic cells | Mature squamous cells |
| Nuclei |
Enlarged up to 1.5 times Binucleation/ multinucleation may be present Nuclear membranes smooth |
Variable enlargement -slight to marked Binucleation/ multinucleation may be present Nuclear membranes smooth |
Enlarged 3-4 times Binucleation/ multinucleation may be present with HPV Nuclear membranes smooth to slightly irregular |
| Chromatin |
Finely granular, evenly distributed Hyperchromasia not evident |
Finely granular, evenly distributed Hyperchromasia not evident |
Finely to coarsely granular, evenly distributed Slightly hyperchromatic |
| Nucleoli | Small and often multiple, uniform | Small to conspicuous and often multiple | Inconspicuous or absent |
| Cytoplasmic Presentation | Peri-nuclear halos often present, small, multiple vacuoles may be evident due to degeneration | Vacuolated cytoplasm with loose tissue culture presentation | Dense, polygonal shape with or without clear, well defined HPV cavitation and a peripheral dense rim of cytoplasm |
- Austin RM: Follow-up of Abnormal Gynecologic Cytology. A College of American Patholgists Q-Probes Study of 16,312 Cases from 306 Laboratories. Arch Pathol Lab Med 2000;124(8):1113-4
- Carpenter AB, Davey D: ThinPrep Pap Test: performance and biopsy follow-up in a university hospital. Cancer 1999;41:39-44.
- DeMay RM: The Art and Science of Cytopathology. Chicago: ASCP Press; 1996
- Diaz-Rosario LA et al: Performance of a fluid-based, thin-layer Papanicolaou smear method in the clinical setting of an independent laboratory and an outpatient screening population in New England. Arch Pathol Lab Med 1999; Sep 123(9):817-21.
- Grace, A, et al: Comparative study: Conventional cervical and ThinPrep Pap Tests in a routine clinical setting. Cytopathol 2002;13:200-05.
- Guidos BJ, Selvaggi SM: Use of the ThinPrep Pap Test inclinical practice. Diagn Cytopathol 1999;20:70-73.
- Lee KR et al: Comparison of conventional Papanicolaou smears and a fluid-based, thin-layer system for cervical cancer screening. Obstet Gynecol 1997;90:278-284.
- Luthra, UH, et al: Performance of monolayered cervical smears in a gynecology outpatient setting in Kuwait. Acta Cytol 2001; 46(2):303-10.
- Weintraub J, Morabia A: Efficacy of a liquid-based thin layer method for cervical cancer screening in a population with a low incidence of cervical cancer. Diagn Cytopathol 2000 Jan;22(1):52-9.