GYN Atlas - Atypical Squamous Cells
SQUAMOUS CELLS
ATYPICAL SQUAMOUS CELLS
Richard A. Smith, MD, PhD
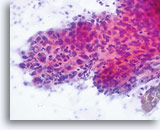
No diagnostic classification causes more debate than Atypical Squamous Cells (ASC). New terms rose from the revised classification of The Bethesda System (TBS) in 2001 and remain for TBS 2014. TBS indicates that the ASC category should be the diagnostic consideration when squamous abnormalities are present that are more marked than those attributable to reactive changes, but fall qualitatively or quantitatively short of the diagnostic criteria for a low grade or high grade squamous intraepithelial lesion. Furthermore, TBS stresses the importance of qualifying this diagnosis as “undetermined significance” (ASC-US) or “cannot exclude HSIL.” (ASC-H)
The proper classification of ASC challenges the cytotechnologist and pathologist and, writing any chapter describing the morphologic criteria of ASC is challenging, given the subjectivity of this interpretation. Since the adoption of TBS, laboratory professionals interpreting the conventional Pap smear may have used this category as a “catch all” for smears that are difficult to classify.
Artifacts inherent to the conventional Pap smear, such as air-dried or partially obscured cells, may result in an ASC diagnosis. The degree of apparent atypia in reactive cells may also be exaggerated by air-drying or smearing. These issues result in the artifacts that make it difficult for the cytotechnologist and pathologist to adequately visualize the nuclear detail of the cells in question, resulting in a less than definitive diagnosis.
The immediate wet fixation that is used in the ThinPrep process may allow the pathologist and cytotechnologist to move away from the ASC “catch all” and better differentiate between cellular changes due to reactive conditions, definitive squamous atypia, and dysplastic lesions. This is not to say that ASC interpretations are eliminated by the adoption of the ThinPrep Pap Test, but the laboratory staff has the opportunity to refine their morphologic criteria, eliminating certain “ASC” cases arising from poor preparation, and better identifying cases that may
harbor abnormality.
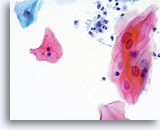
The ThinPrep Pap Test® minimizes the troublesome artifacts inherent in smear and spray fixation. This allows for
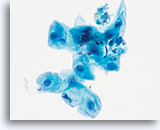
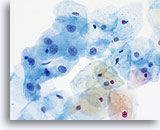
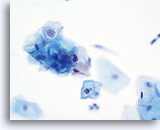
the nucleus to be adequately visualized facilitating a more definitive diagnosis. The epithelial cells that are generally incorporated in the ASC category are the mature squamous and squamous metaplastic cells exhibiting changes that are minimal and fall short of a diagnosis of LSIL or HSIL. The nuclei are slightly enlarged and this enlargement is compared to the normal entity of the same cell type. The nuclei may show slight nuclear membrane irregularities but are more often smooth. When dealing with the metaplastic component, one needs to make sure that the irregularities aren’t due to a vacuole(s) pushing the nucleus into the aberrant shape. The chromatin pattern is finely granular and evenly distributed. Chromocenters or nucleoli are generally inconspicuous or absent unless a reactive process is occurring in conjunction with the atypia at which point the differential diagnosis of reactive needs to be considered depending upon the presence or lack of the other criteria.
With either conventional or ThinPrep® slides, an ASC interpretation may arise from any of several different cellular changes, including but not limited to, squamous atypia, atypical squamous metaplasia, and atypical parakeratosis. The criteria for ASC on the ThinPrep Pap Test are as follows:
LOOK-ALIKE ENTITES:
| REACTIVE | ASC-US | LSIL | |
| Nucleus | Enlarged 1.5-2 times,flat | Enlarged 2 -3 times, flat to minimal depth of focus | Enlarged 3-4 times,Slight depth of focus |
| Nuclear Membrane | Smooth | Smooth to slightly irregular | Smooth to slightly irregular |
| Chromatin | Finely granular, evenly distributed | Finely granular, evenly distributed | Slightly more granular, evenly distributed |
| Nucleoli/Chromocenters | Small to conspicuous, sometimes multiple | Inconspicuous or absent | Absent |
| Cytoplasmic Features | Peri-nuclear halos present | Questionable cavitations | Diagnostic HPV cavitations |
| Bichromasia | Can be present | Not present | Not present |
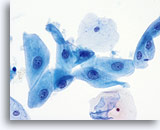
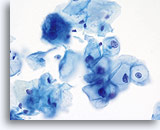
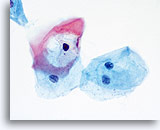
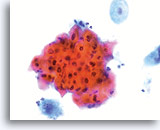
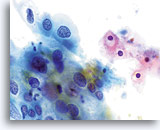
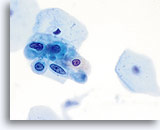
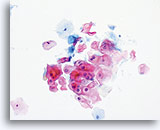
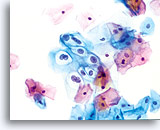
The images that follow are ThinPrep® Pap Test specimens that reasonably could be interpreted as reactive changes,
ASC-US, and LSIL.
As previously mentioned, ASC will not be eliminated by the adoption of the ThinPrep® Pap Test. In fact, the better cellular preservation that is afforded by liquid fixation can lead to over interpretation of nuclear size and chromatin as ASC if one is not familiar with the consequences of liquid fixation as discussed in the introductory material regarding “microscopic evaluation of ThinPrep slides”. There are circumstances where laboratory staff may transiently experience an increase in their use of ASC classification immediately after adoption of the ThinPrep Pap Test, then, after gaining experience, see that rate drop below that which was experienced with the conventional Pap.
ASC, as long as it remains a category in TBS, will be used by pathologists because of inherent subjectivity of human diagnosis, and variable interpretation of criteria. Also important is the biologic nature of Human Papilloma Virus (HPV) that causes morphologic perturbations in cells that are less than LSIL. The morphologic changes caused by HPV are discussed in greater detail in the section covering Low Grade Squamous Intraepithelial Lesions. The role of this virus in the causation of ASC has created the opportunity to determine the relative risk of ASC changes by the determination of high- vs. low-risk types of virus through ancillary testing of the material in the ThinPrep Pap Test vial.
- Crum CP et al: Subclassifying atypical squamous cells in ThinPrep cervical cytology correlates with detection of high-risk human papillomavirus DNA. Am J Clin Pathol 1999; 112:384-90
- Dziura B et al: Improved ASCUS diagnosis: Clinical and financial implications for follow-up care. Ob, Gyn. News 1999; 1:12-13
- Ferenczy et al: Diagnostic performance of Hybrid Capture human papilloma virus deoxyribonucleic acid assay combined with liquid-based cytologic study. Am J Obstet Gynecol 1996;175(3 pt.1): 951-6.
- Ferris et al for the Atypical Squamous Cells of Undetermined Significance/Low-Grade Squamous Intraepithelial Lesions Triage Study (ALTS) group: Cervicography for triage of women with mildly abnormal cervical cytology results. Am J Obstet Gynecol 2001;185(4):939-43.
- Hong et al: Comparative analysis of a liquid based Pap test and concurrent HPV DNA assay of residual samples. ACTA Cytol 2002;46(5):828-34.
- Lin WM et al: Molecular Papanicolaou tests in the twenty-first century: Molecular analyses with fluid-based Papanicolaou technology. Am J Obstet Gynecol 2000; 39-45
- Manos MM et al: Identifying women with cervical neoplasia: Using human papillomavirus DNA testing for equivocal Papanicolaou results. JAMA 1999; 281:1605-10
- Papillo J et al: Evaluation of the ThinPrep Pap Test in clinical practice: a seven-month 16,314 case experience in northern Vermont. Acta Cytologica 1998; 42:204-208
- Quddus et al: Atypical squamous metaplastic cells: Reproducibility, outcome, and diagnostic features on ThinPrep Pap Test. Cancer (Cancer Pathol) 2001:93:16-22.
- Quddus et al: Utility of HPV DNA detection in thin-layer, liquid-based tests with atypical squamous metaplasia. ACTA Cytol 2002;46(5):808-12.
- Sherman et al: Cervical specimens collected in liquid buffer are suitable for both cytologic screening and ancillary human papillomavirus testing. Cancer 1997;81:89-97.
- Sherman et al: Performance of liquid based , thin-layer cervical cytology: Correlation with reference diagnosis and human papilloma virus testing. Mod Pathol 1998;11:837-843.
- Wright et al for the ASCCP-sponsored Consensus Conference: 2001 consensus guidelines for the management of women with cervical cytologic abnormalities. JAMA 2002;287(16):2120-29.