GYN Atlas - Endometrial Adenocarcinoma
EPITHELIAL CELL ABNORMALITIES
ENDOMETRIAL ADENOCARCINOMA
Luis A. Diaz-Rosario, MD
Endometrial adenocarcinoma is the most common gynecologic malignancy, accounting for more than two thirds of the uterine corpus cancers. Clinically it is divided into two types. Type I, which represent 2/3 of endometrial adenocarcinomas, usually arises in premenopausal or perimenopausal women with a clinical history of endogenous or exogenous hyperestrogenic states. These usually evolve through a neoplastic process that extends from hyperplasia to well-differentiated invasive adenocarcinoma, and are usually responsive to hormonal therapy with a better prognosis than the Type II malignancies. Type II, which represent 1/3 of endometrial adenocarcinomas, usually affect postmenopausal women, are not associated to hyperestrogenic states and usually present themselves as poorly differentiated neoplasms. Some women with either well-differentiated or poorly differentiated adenocarcinoma of the endometrium can be diagnosed when cells are collected from the cervix for Pap smear examination. As with the conventional Pap smear, the cytologic presentation of endometrial adenocarcinoma on ThinPrep® Pap Test slides depends largely on the grade and type of the neoplasm. Since endometrial lesions are not sampled directly for a Pap test, higher-grade neoplasms will tend to exfoliate more cells and be more evident. The uniform distribution and liquid fixation of cells in ThinPrep Pap Test samples may aid in the detection of well-differentiated lesions, which usually present with a low number of abnormal cells, and early, subtle cellular changes.
Patient history, although important in all aspects of cytology, is extremely important when dealing with endometrial cells on the Pap test. The patient’s age and history may play a large role in diagnosing benign, atypical and frankly malignant endometrial cells. Well-differentiated endometrial adenocarcinoma can be cytologically difficult to distinguish from benign endometrium and endometrial hyperplasia and further studies and publications would be helpful to further define these criteria.
The degree of atypia in endometrial adenocarcinoma increases with tumor grade. The cells can vary from appearing benign to frankly malignant and for purposes of classic criteria, we will describe the frankly malignant features to be used as a base guideline for cytologic use.
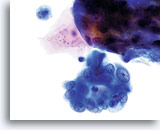
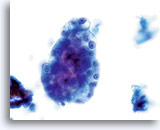
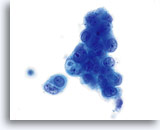
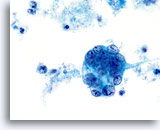
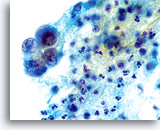
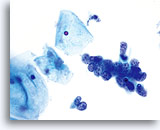
Cytologically, Type I neoplasms show atypical/malignant endometrial cells upon an increased maturation index background. By contrast, Type II neoplasms usually show upon an atrophic background. On ThinPrep samples the endometrial cells will be well preserved and may appear in 3-dimensional crowded groupings of varying sizes as well as small flat sheets containing few cells. The cells usually appear larger than their normal counterpart and the groups have smooth, sometimes scalloped borders giving them a papillary configuration. The cytoplasm is finely to discretely vacuolated and some larger vacuoles can be observed compressing the nucleus to one side of the cell as well as occasionally exhibiting polymorphonuclear cell engulfment. Nuclear features vary dependent upon the grade of the tumor. In general, as the tumor becomes less differentiated, the nucleus tends to round up with an associated gradual increase in nuclear area (µm2), size and number of nucleoli, irregularities in the distribution and coarseness of the chromatin and thickening of the nuclear membranes.
The cytologic criteria for endometrial adenocarcinoma on the ThinPrep® Pap Test are as follows:
Polymorphonuclear cells may be engulfed in the cytoplasm. 60x
Overall cell size is usually larger than the normal counterpart. 60x
Nuclei “round up” compared to the normal nucleus. 60x
Nuclear membranes may be thickened. 60x
Chromatin may be clumped and irregularly distributed. 60x
Nucleoli are common and vary in frequency, size and number. 60x
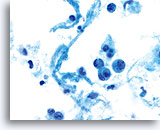
The contextual clues found in the background of these lesions are maintained when utilizing the ThinPrep® Pap Test. Tumor diathesis most commonly found in the form of a watery diathesis on the conventional Pap smear presents as granular, clumped debris on Thin Prep® Pap Test, thereby not obscuring the cellular detail.
Tumor diathesis and single malignant cells may be noted. 60x
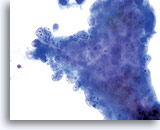
Tumor diathesis may be present and appears as a “woven shroud” with a denseness or linear presentation of debris in the center and a frayed or pulled out appearance of the material around the edges of the group. 60x
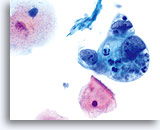
LOOK-ALIKES
Endometrial adenocarcinoma has a few look-alike entities although the age and history of the patient may help with the differential diagnoses. Endometrial adenocarcinoma, specifically endometrioid type, may resemble endocervical adenocarcinoma. It can have a sheet like appearance rather than a total overall papillary presentation. Endometrioid adenocarcinoma can be difficult to discern if it is primary to the uterus and growing down into the cervix or vice versa.
The small cell type of squamous cell carcinoma is another potential look-alike for endometrial adenocarcinoma due to its small cell size and lack of cytoplasm.
Note: Endometrial cells from hyperplasia or atypical hyperplasia may be detected and may be difficult to differentiate from a neoplasm. (See section on AGC)
| ENDOMETRIAL ADENOCARCINOMA | ENDOCERVICAL ADENOCARCINOMA | SMALL CELL SQUAMOUS CARCINOMA | |
| Tissue Presentation | Small, loose clusters, cell balls (3 dimensional clusters), and large sheets in poorly differentiated tumors | Few single cells, strips, rosettes and two dimensional sheets and clusters with well- defined group borders (scalloped edges) | Single cells and aggregates or syncytial-like arrangements are seen. Tissue presentation is more flat than clustered. |
| Cytoplasm | Finely to discretely vacuolated with some large vacuoles, N/C ratio 2:1 to very scant cytoplasm | Finely vacuolated with occasional single discrete vacuole, N/C ratio 2:1 | Cytoplasm is scant and finely vacuolated or delicate. |
| Nucleus | Slightly enlarged to enlarged (slightly larger than intermediate cell nucleus), predominantly round to oval | Enlarged (3-4 times larger than intermediate cell nucleus), round to oval | Nuclei are generally round to oval and occupy up to 95% of the cytoplasm. Pyknotic forms may be seen |
| Nuclear Membrane | Smooth, thickened | Smooth to irregular (undulating), thickened | Nuclear membranes are smooth to irregular and are thickened |
| Chromatin | Coarse, unevenly distributed with parachromatin clearing, slight hyperchromasia | Coarse, granular and hyperchromatic (stealth gray chromatin) | Coarse and hyperchromatic although some can appear finely granular, evenly distributed |
| Nucleoli | Single to multiple, regular, not in every cell | Numerous, prominent, smooth to irregular, single to multiple | Nucleoli are often present and are small and sometimes multiple |
Endometrial adenocarcinoma 60x
Endocervical adenocarcinoma 60x
Small cell carcinoma 60x
- DeMay RM: The Art & Science of Cytopathology. Chicago, IL. ASCP Press, 1996, pp 122-127.
- Guidos BJ et al: Detection of endometrial adenocarcinoma with the ThinPrep Pap test. Acta Cytol 1999; 43(5): 903.
- Johnson JE et al: Endocervical glandular neoplasia and its mimics in ThinPrep Pap tests. A descriptive study. Acta Cytol 1999;43(3):369-75.
- Papillo J et al: Increased specificity in the detection of glandular lesions: Decreased false positive AGUS with ThinPrep Pap tests. Acta Cytol 1999; 43(5): 902.
- Tao L-C: Cytopathology of the Endometrium Direct Intrauterine Sampling. Chicago, IL. ASCP Press, 1993, pp 71-107.