GYN Atlas - Negative for Intraepithelial Lesion or Malignancy
Negative for Intraepithelial Lesion or Malignancy
Jacalyn L. Papillo, BS, CT(ASCP) & Pamela Smith Piraino, CT(ASCP)
The Bethesda 2014 diagnostic category of Negative for Intraepithelial Lesion or Malignancy encompasses a wide variety of benign conditions that represent a broad spectrum of morphologic changes. The common denominator is that the changes lack features necessary for a diagnosis of Atypical Squamous Cells — Undetermined Significance or more severe conditions. Factors such as age, the date of last menstrual period, hormonal influences, presence of infectious agents, prior atypia or treatment for atypia may influence the cytologic presentation of cells. Pertinent clinical information is important and should be taken into consideration when rendering a diagnosis.
Whether utilizing the ThinPrep Pap Test or the conventional Pap smear, it is essential to have a firm understanding of what constitutes “normal”. The ThinPrep process does not significantly alter the cytologic presentation of normal squamous and endocervical cells, as seen from the photomicrographs in the previous chapter on specimen adequacy. However, further discussion is warranted in the following areas: atrophy, pregnancy, post-partum changes, cytolysis, tubal metaplasia, lower uterine segment and benign appearing endometrial cells.
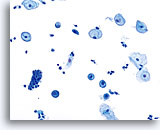
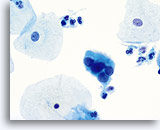
Atrophy
With the progression of atrophy during perimenopause and menopause there is a thinning of the epithelium, which often leads to a corresponding decrease in the number of cells shed during sample collection. Cell maturation is retarded, so that the prominent cell type becomes parabasal. With this shift in hormonal status the cell sample may contain increased glycogen, cellular degeneration and stripped nuclei. A granular background of degenerative cellular debris is generally seen. An inflammatory response is often present and evidence of bleeding is sometimes appreciated. Slight changes in the nuclear contours of the parabasal cells due to degeneration could lead to an over-diagnosis of atypia. It is important to evaluate nuclear size, the nuclear to cytoplasmic ratio and chromatin pattern carefully before rendering a cytologic diagnosis of ASC-US or more severe lesion in atrophic smears. In the case of atrophy with co-existing SIL, a sub-population of atypical cells should exhibit increased N/C ratios, hyperchromasia and irregular nuclear membranes.
Pregnancy
The cytologic patterns associated with excessive hormonal influences, such as pregnancy, are similar with conventional Pap smears and ThinPrep slides. During pregnancy, caution should be used to properly differentiate glycogenated cells from true koilocytes present with HPV-associated changes. This can be done by noting a lack of nuclear irregularity, along with a smooth round vacuolization from glycogen, compared to abnormal nuclei surrounded by a sharp irregular cavitation caused by HPV.
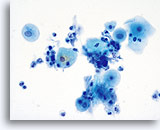
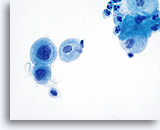
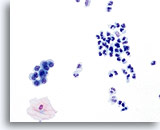
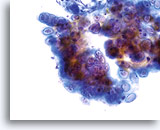
Postpartum Changes
During the postpartum period, or if breast feeding, a hormonal pattern of low squamous maturation predominates. Parabasal cells are abundant, usually presenting singly. Glycogen may also be present. A background of inflammatory cells and reactive changes is often present and may require additional scrutiny. Adherence to strict cytologic criteria (the lack of an increased N/C ratio, abnormal chromatin and irregular nuclear membranes) should preclude an over-diagnosis of cytologic atypia.
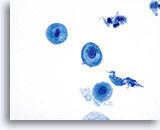
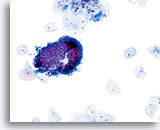
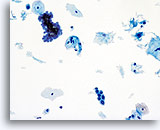
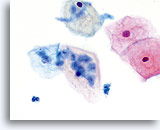
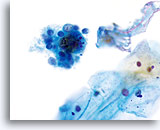
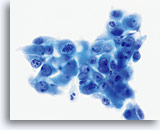
Postpartum
High power view of parabasal cells during postpartum. Note presence of glycogen and low N/C ratio. 60X
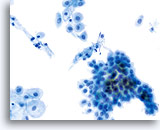
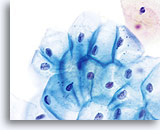
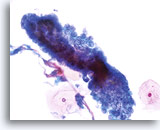
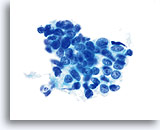
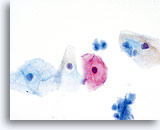
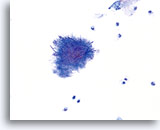
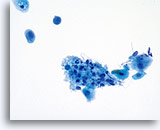
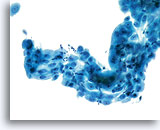
Postpartum
HSIL in a postpartum sample. Note the increased N/C ratio and abnormal chromatin in the HSIL cells as compared to the parabasal cells, apparent even at low magnification.
20X
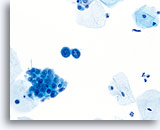
Cytolysis
The familiar pattern of bare nuclei, superficial and intermediate cells and Döderlein bacilli associated with lactobacilli-induced cytolysis can be readily identified at low magnification on ThinPrep slides. The bacilli may be trapped in mucus or seen overlying squamous cells.
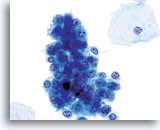
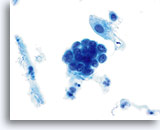
Tubal Metaplasia
Tubal metaplasia is characterized by columnar cells with pleomorphic, hyperchromatic nuclei with increased N/C ratios. As with conventional Pap smears, cells from tubal metaplasia may occasionally be mistaken for atypical endocervical cells and even adenocarcinoma in situ. In order to avoid an over-diagnosis, look for the presence of discrete cytoplasmic vacuoles, terminal bars and cilia.
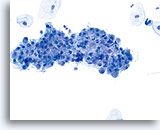
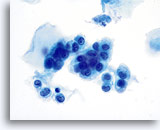
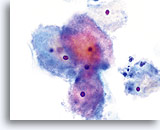
Lower Uterine Segment
With increased vigilance by providers to collect adequate specimens, aggressive sampling may result in the presence of cells from the lower uterine segment in cervicovaginal samples. Cells from the lower uterine segment generally present as a tissue fragment rather than individual cells or small groups of cells. The fragment has well ordered nuclei and nucleoli may be present. A folding over of the fragment on itself may cause a three dimensional appearance.
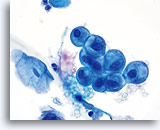
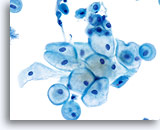
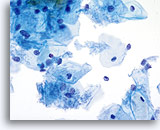
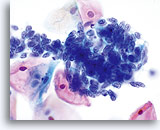
Benign Appearing Endometrial Cells
Endometrial cells may display a wide range of nuclear and cytoplasmic size, as well as architectural configuration. Endometrial cell groups tend to round up in ThinPrep solution. The nuclei are well preserved and appear crisp with distinct, active chromatin; chromocenters are frequently noted.
Bethesda 2014 recommends the reporting of benign appearing exfoliated endometrial cells in women age 45 and above, regardless of clinical history. The general categorization “Other” was included in the Bethesda 2001 lexicon for this purpose. Histiocytes, stromal cells and abraded endometrial cells do not have the same significance as exfoliated endometrial cells and should not be considered in the same context. While most often benign, identification of endometrial cells, particularly if not associated with menses or after menopause, may indicate risk for an endometrial abnormality.
ORGANISMS AND OTHER NON-NEOPLASTIC FINDINGS
All pathogens commonly found on the conventional Pap smear are easily identified on ThinPrep slides because their morphology and visualization of their associated cellular changes are often optimized by the immediate wet fixation protocol utilized with the ThinPrep process. Contextual clues and patterns are maintained through specimen processing and are identifiable when screening ThinPrep slides.
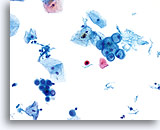
Trichomonas Vaginalis
On ThinPrep slides, trichomonads may appear slightly smaller than the air dried organisms found on the conventional Pap smear. Because of the rapid fixation, the ThinPrep Pap test slides bear a similarity to a “wet prep” used in the physician’s office.
Although proportionately smaller, the organisms maintain their characteristic internal structure and often retain their flagellae lending confidence to the diagnosis. Two findings characteristically found on ThinPrep slides are useful in the detection of T. Vaginalis: trichomonads tend to present either as isolated organisms or in prominent groupings, or microcolonies, often overlying epithelial cells or clustering together.
Candida species
The spearing of the epithelial cells with the cells folding along the long axis of the organism is the first clue that Candida spp. is present on the ThinPrep slide. Pseudo-septate hyphae and budding yeasts are preserved and easily detected. Staining may vary from colorless to eosinophilic to gray-brown depending upon patient biology. Laboratories often observe an increased detection of Candida spp. when implementing the ThinPrep Pap Test.
Herpes Simplex Virus
The classic characteristics of herpes virus infection are retained and readily identified on ThinPrep slides. Cellular changes such as multi-nucleation, nuclear molding, ground-glass chromatin, chromatin margination, and intranuclear viral inclusions aid in the diagnosis.
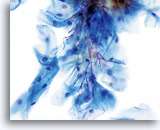
Actinomyces
Delicate and dense branches of filamentous bacteria with accompanying sulphur granules allow for easy identification of the organism. Infection by Actinomyces often accompanies the use of an intrauterine device (IUD) or a pessary.
IUD Changes
Patients with an IUD may occasionally show single or clustered glandular cells with an increase in nuclear to cytoplasmic ratio. Nucleoli may be present and prominent vacuoles may cause a signet ring appearance to the cells. To avoid a diagnosis of AGUS, cellular changes must be correlated with patient history. These changes often accompany an infection with Actinomyces.
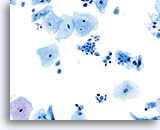
Shift in the Flora Suggestive of Bacterial Vaginosis
Squamous cells may be covered with coccobacilli when the normal lactobacilli are absent. A diagnosis of bacterial vaginosis may be confirmed by bacterial culture.
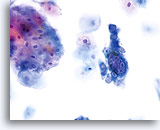
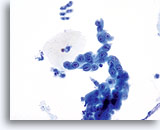
Chronic Follicular Cervicitis
The presence of lymphocytes accompanied by tingible body macrophages may indicate a chronic inflammatory condition or the rupturing of a lymph follicle during sample collection. On the ThinPrep slide the lymphocytes from chronic follicular cervicitis will generally appear in small clusters grouped together. The presence of tingible body macrophages aid in the diagnosis.
Radiation
The same changes found on conventional Pap smears following radiation therapy are seen on the ThinPrep Pap Test slides. Cells may be enlarged, show multinucleation, vacuolization, bi-chromasia, and altered chromatin. Ingested inflammatory cells may also be present.
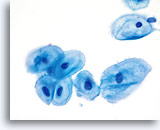
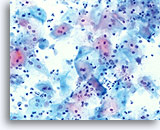
Atrophy with inflammation
Conventional Pap smears from atrophic patients generally contain a uniform background of granular debris, and degenerated inflammatory cells. With ThinPrep slides this background debris is maintained, but is often pooled into small clumps alongside atrophic epithelium.
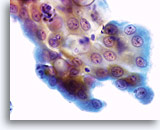
Decidual changes
The cells of patients who are late in their pregnancy (or postpartum) may show changes which can mimic high grade dysplasia. The morphologic characteristics of decidual change on ThinPrep Pap test slides are similar to those found on the conventional Pap smear.
Repair
Criteria to classify a reparative process on Thin Prep slides are similar to the criteria as enumerated in The Bethesda System.
- Minimal nuclear enlargement (11/2 to 2 times normal intermediate cell nucleus)
- Bi and multi-nucleation may occur
- Mild hyperchromasia may be present
- Chromatin finely granular, evenly distributed
- Karyopyknosis and karyorrhexis may occur
- Nuclear membranes smooth
- Prominent single or multiple nucleoli
- Flat sheets with polarity maintained; groups may round up in fluid
- Mitosis and single cells may be noted
- Often accompanied by neutrophils, inflammatory changes and/or organisms
- Biscotti CV, et al: Thin-layer Pap test vs conventional Pap smear: Analysis of 400 split samples. J Reprod Med 2002;47(1):9-13.
- Lee KR, et al: Comparison of conventional Papanicolaou smears and a fluid-based, thin-layer system for cervical cancer screening. Obstet Gynecol 1997;90:278-284.
- Solomon, Diane, et al: The 2001 Bethesda System, terminology for reporting results of cervical cytology, JAMA 2002;287(16): 2114-2119.