Radiation Gallery
Discussion
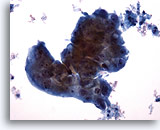
Radiation treatment of malignant lesions in the female genital tract traumatizes the epithelium causing ulceration that can cytologically mimic dysplasia or carcinoma. The extent of this trauma depends on the type and duration of therapy, therefore the cellular changes may resolve within six months or can persist for a lifetime. Some chemotherapeutic agents can also produce similar cellular changes, making patient history a valuable tool. Post-radiation dysplasia (PRD) has been reported in up to 23% of patients with the atypia resembling that of non-radiated patients. Considering the difficulties in distinguishing PRD from recurrent carcinoma, colposcopy and biopsy are recommended to rule out the latter.
Cytology
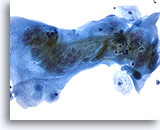
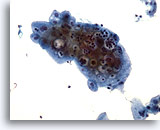
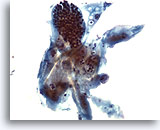
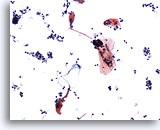
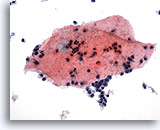
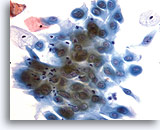
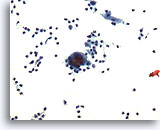
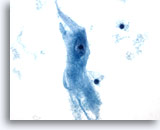
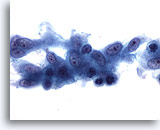
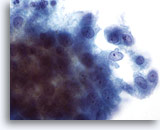
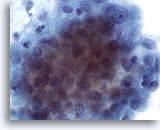
Cytomegaly is the most well known radiation related change. Cytomegalic cells have enlarged and/or multiple nuclei and abundant cytoplasm while maintaining a fairly normal N/C ratio. The nuclei can be pale and the chromatin can be finely granular to “smudgy” with possible micro- and macronucleoli and vacuoles. The cytoplasm may exhibit bichromasia and vacuoles with or without engulfed polys. Bizarre cell shapes may also be seen. The background of these specimens will contain degenerated blood that appears “stringy”, cellular debris, polys and histiocytes. Reparative changes can be seen frequently and occur in single-layered, cohesive, streaming sheets with pale nuclei and prominent nucleoli. Radiated fibroblasts are present and have delicate cytoplasm with vacuoles and cytoplasmic projections. The nuclei are pale, finely granular with possible nucleoli. Degenerated tumor cells may be seen in specimens initially following radiation.
References
- Atkinson/Silverman: Atlas of Difficult Diagnoses in Cytopathology, 1998: 32, 57, 69, 79, 105.
- DeMay, R: Practical Principles of Cytopathology, 1999: 17.
- Nguyen/Kline: Essentials of Exfoliative Cytology, 1992: 101-108.