GYN Atlas - Endocervical Adenocarcinoma
EPITHELIAL CELL ABNORMALITIES
ENDOCERVICAL ADENOCARCINOMA
Raheela Ashfaq, MD
The cells of endocervical adenocarcinoma as represented on the ThinPrep® Pap Test are well preserved and maintain the classic glandular structures and arrangements as observed in other liquid based collection methods, ie: adenocarcinoma in body-fluid non-gynecologic samples. The diagnosis of adenocarcinoma has taken on greater significance in recent years, due to both a relative, and absolute increase in its incidence. Unfortunately, this diagnosis is often difficult in conventional samples of the cervix, owing to incomplete sampling of the endocervical canal or poor preservation of glandular material.
Correctly diagnosing endocervical adenocarcinoma will greatly depend on the grade of the invasive lesion as well as the presence or absence of a tumor diathesis. Well-differentiated lesions can be difficult to distinguish from in-situ lesions and often times the definitive diagnosis is determined on the surgical biopsy specimen. Because of the rapid fixation techniques employed with the ThinPrep Pap Test, primary emphasis need not be placed on the tissue architecture alone, but on the nuclear features as well. Criteria such as nuclear membrane irregularities and chromatin patterns are important to assist the cytologist in differentiating neoplastic glandular lesions from a benign reparative process. The absence of air-drying results in a clearer view of the nuclear features and eliminates the smudged chromatin staining thereby making the diagnosis less difficult.
As with other diagnostic entities, a range of glandular disease may accompany the adenocarcinoma in the form of AIS. Continuing to screen for the most severe presentation of the lesion is an important factor in a high rate of biopsy correlation in the laboratory.
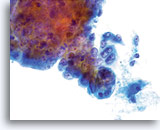
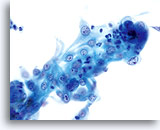
An accurate diagnosis of endocervical adenocarcinoma is easiest when there has been adequate sampling of the lesion, resulting in numerous sheets and groups of atypical cells easily visualized at screening magnification. The classic criterion of two-dimensional sheets and groups are present and these groups begin to round up and exhibit less of the glandular differentiation observed in AIS in the form of strips, pseudostratification and crowding. The three-dimensional clusters may exhibit scalloping around the edge of the group with the nucleus protruding out into the cytoplasm and poly engulfment can also be seen (this feature is not exclusive to either endocervical or endometrial lesions).
Nuclear morphology of endocervical adenocarcinoma varies with the differentiation of the lesion. Well-differentiated nuclei exhibit finely granular, hyperchromatic, evenly distributed chromatin most closely resembling the nuclei of AIS. As the lesion progresses, the nuclei appear more and more atypical. The nuclei are enlarged, taking up 2/3 or more of the cytoplasm. The chromatin becomes more coarse and often times becomes irregularly distributed and exhibits parachromatin clearing. Nuclear membrane irregularities are also present although they tend to be undulating and smooth rather than having the “bites” and “divot holes” seen in squamous lesions. Macronucleoli may be present and can be irregular in their presentation. A necrotic tumor diathesis and/or blood may be present and along with the cellular features, will assist in making the diagnosis of an invasive lesion.
The cytologic criteria for Endocervical Adenocarcinoma are as follows:
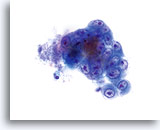
Glandular cell clusters round up in PreservCyt solution and may exhibit scalloping around the edges of the group. Note the smooth, distinct cytoplasmic borders to the edge of the group.
40x
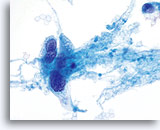
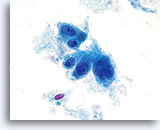
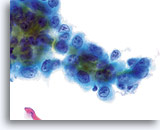
Poly-engulfment can be seen in endocervical adenocarcinoma as well as in endometrial adenocarcinoma.
60x
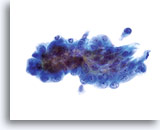
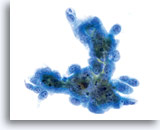
Nuclei are enlarged, often occupying more than 2/3 of the cytoplasm and generally remain round to oval with undulating nuclear membranes.
60x
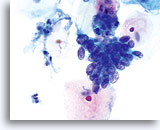
Nuclear membranes are thickened and nuclear membrane irregularities are undulating as opposed to the “rat bite” membranes seen in squamous lesions.
40x
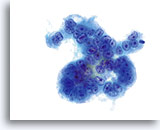
Chromatin patterns vary from fine to coarsely granular and can appear evenly distributed although coarse and clumped. Nuclei appear hyperchromatic and exhibit a greater depth of focus as compared to the normal entity.
60x
Parachromatin clearing may be evident and the nuclei will exhibit a greater depth of focus as compared to the normal endocervical component nuclei.
60x
Nucleoli, when present are prominent and often multiple and irregular.
60x
Tumor diathesis may be present and appears as a “woven shroud” with a denseness or linear presentation of debris in the center and a frayed or pulled out appearance of the material around the edges of the group.
60x
Cells of endocervical adenocarcinoma may be accompanied by ghost red blood cells.
60x
LOOK-ALIKES*
| ENDOCERVICAL ADENO- CARCINOMA |
ADENOCARCINOMA IN-SITU | ENDOCERVICAL REPAIR | SQUAMOUS CELL CARCINOMA (INVOLVING GLANDS) | |
| Tissue Presentation | Few single cells and two dimensional sheets and clusters with well-defined group borders (scalloped edges) | Strips of glandular epithelium exhibiting pseudo-stratification, with feathering, rosettes, few single cells | Flat sheets of epithelium | Definitive squamous component, sheets of poorly defined epithelium with foamy cytoplasm and no definitive glandular differentiation |
| Cytoplasm | Finely vacuolated with pre- dominantly multiple discrete vacuoles, N/C ratio 2:1 |
Vacuolated, maintain some columnar dif- ferentiation, N/C ratio increased | Abundant, “tissue culture” appearance, N/C ratio low | Finely vacuolated, no discrete vacuoles, ill-defined cytoplasm at group edges (frayed appearance) |
| Nucleus | Enlarged, round to oval | Enlarged, oval to elongate | Variable in size within group, round | Variable, round to oval |
| Nuclear Membrane | Smooth to irregular (undu- lating), thickened |
Smooth to slightly irregular | Smooth | Smooth to irregular, (bites and divots) |
| Chromatin | Coarse, unevenly distributed, para-chromatin clearing, greater depth of focus | Finely granular, evenly distributed, hyper chromatic, increased depth of focus |
Finely to coarsely granular, evenly distributed, hypo- chromatic, flat focus |
Finely granular, evenly distributed, greater depth of focus |
| Nucleoli | Large, prominent, smooth to irregular, single to multiple | Indistinct to moderate in size and regular | Small, sometimes multiple, in every nucleus | Absent to occasional, small |
* The reader must take note that the criteria mentioned above is for the classic appearance of each diagnostic entity and that these entities may overlap in their criteria making a definitive diagnosis more difficult. These criteria are meant to be used as a guideline for base line criteria allowing for a range of epithelial appearances and diagnostic thresholds to be taken into consideration.
Endocervical adenocarcinoma
40x
Adenocarcinoma in situ
60x
Endocervical repair
40x
Squamous cell carcinoma with gland neck involvement
60x
- Ashfaq R et al: ThinPrep Pap Test accuracy for glandular disease. Acta Cytol 1999;43: 81-85.
- Bai H et al: ThinPrep® Pap Test promotes detection of glandular lesions of the endocervix. Diag Cytopathol 2000; 23 (1): 19-22.
- Johnson JE and Rahemtulla A: Endocervical glandular neoplasia and its mimics in ThinPrep Pap Tests. A descriptive study. Acta Cytol 1999; 43(3): 369-75.
- Roberts JM et al: Comparison of ThinPrep and Pap Smear in relation to prediction of Adenocarcinoma In Situ. Acta Cytol 1999 Jan-Feb:43(1):74-802
- Smith HO et al: The rising incidence of adenocarcinoma relative to squamous cell carcinoma of the uterine cervix in the United States – A 24-year population-based study. Gynecol Onc 2000; 78, 97-105