Case Presentation
Case Presentation – July 2022
Metastatic Hepatocellular Carcinoma
Written by: Sydnee Webb, Student, Cleveland Clinic School of Cytotechnology, Cleveland, OH
Patient Age: 67 years old, Male
Specimen Type: 11L Lymph node, Traditional smear with Diff-Quik, ThinPrep® Non-Gyn, Cell Block
Patient History: Hepatocellular carcinoma, liver transplant, PET-positive lung nodule
Cytologic Diagnosis: Positive for malignant cells, metastatic carcinoma
Biopsy / Pathologic Diagnosis: Metastatic carcinoma
Case provided by: Cleveland Clinic
Metastatic Hepatocellular Carcinoma
Etiology:
Hepatocellular carcinoma (HCC) is the most common type of primary liver cancer1 and is the second leading cause of cancer-related deaths globally.2 HCC tumors originate from mature hepatocytes or progenitor cells in the liver.3 Increased risk of HCC is associated with chronic liver damage and cirrhosis which may be caused by alcohol abuse, chronic Hepatitis B or C infection, tobacco use, aflatoxin exposure, obesity, diabetes, liver disease, and diet.2,3 HCC is most common over the age of 50.1
Extrahepatic metastasis has been reported to occur in 14.0-36.7% of patients with HCC, and metastasis is more likely to occur with a higher stage at initial diagnosis.4 Of all extrahepatic metastases, 47% are reported to occur in the lung.3 HCC recurrence after liver transplant occurs in 8-20% of patients usually within the first two years.5
Clinical Features:
HCC classically presents with right upper quadrant abdominal pain, weight loss, and hepatomegaly. As the disease advances, weight loss, fatigue, and anorexia become more common.3 Patients with known cirrhosis, a common precursor of HCC, may present with a decrease in liver function resulting in ascites, variceal hemorrhage, progressive encephalopathy, or jaundice.3 Portal vein thrombosis is a common complication, and around 10% of cases may have GI bleeding.3 Screening programs used more recently for patients with cirrhosis can allow HCC to be diagnosed at the asymptomatic stage and in these cases, the symptoms of HCC overlap with symptoms of cirrhosis.3 On imaging, tumors present as solitary or multiple nodules2 and are characterized as arterial-enhancing lesions.3 Extrahepatic metastases are typically discovered as new lesions in radiological imaging.4
Treatment and Prognosis:
Treatment for primary HCC is dependent on the size of the tumor and number of nodules, its location in relation to major vessels in the liver, the presence of portal vein thrombosis, and the degree of liver fibrosis and damage.3 For patients with mild or no cirrhosis, possible treatments include laparoscopic liver resection, radiofrequency ablation, or microwave ablation.3 Adjuvant chemotherapy isn’t shown to reduce recurrence rates in these cases, but using anti-Hepatitis B therapies may be effective.3 For patients who aren’t candidates for resection, transplantation is usually recommended.3 Some patients with tumors outside the transplant criteria can become eligible for transplant after completing regional therapy that reduces tumor staging.3 Chemotherapy is offered to patients who aren’t eligible for resection or transplant.3 For patients with extrahepatic HCC metastasis to the lung after liver transplant, pulmonary metastases resection can prolong survival.5
Prognosis of HCC varies by tumor characteristics, patient comorbidities, and treatment. Patient outcomes are more favorable in those with few comorbidities and preserved liver function.6 A higher mortality has been observed for patients with alcohol-related HCC than those with Hepatitis B related HCC.6 Primary HCC has an overall five-year survival rate of less than 20%,6 however HCC diagnosed in an early stage and treated with a liver transplant is reported to have a five-year survival rate of over 70%.3 The average 1-year survival rate for patients with extrahepatic metastases in one retrospective study was 24.9%.4
The patient in this case had a history of Hepatitis C infection which caused extensive liver cirrhosis. After diagnosis of HCC, he was not a surgical candidate and was treated with radioembolization, chemoembolization, and sorafenib. This treatment successfully down staged the diagnosis and the patient underwent a liver transplant. Lung nodules were first found on a CT scan four years post-transplant and were found to have increased in size several months later.
Cytology:
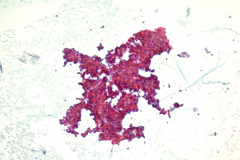
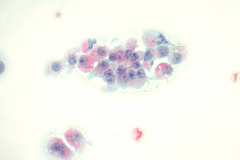
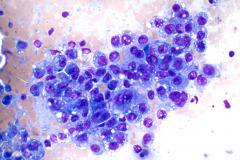
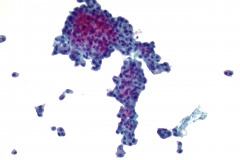
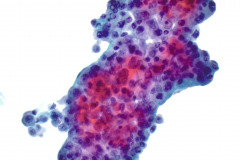
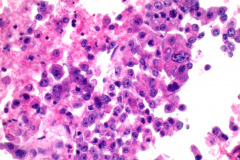
HCC has 3 main patterns: trabecular, pseudoglandular (acinar), and compact.1 Bile is prominent in some tumors, and cytoplasmic inclusions such as Mallory hyaline bodies, globular hyaline bodies, pale bodies, and ground glass are possible.1 HCC can present in a wide range of appearances, from poorly to well differentiated.1 Well differentiated HCC is highly cellular with an architecture that has isolated cells, naked nuclei, trabeculae surrounded by endothelial cells, pseudoglandular structures, transgressing vessels, and irregularly arranged sheets.1 HCC cells can retain benign hepatocellular criteria including polygonal shape, abundant eosinophilic granular cytoplasm, increased nuclear to cytoplasmic ratios, large round nuclei with prominent nucleoli, intranuclear pseudoinclusions, and intracellular bile1. Poorly differentiated HCC tends to be highly cellular with isolated cells or clusters and has pleomorphism, atypical mitoses, giant cells, spindle cells, bile, and less obvious hepatocytic differentiation.1 HCC cells tend to stain positively for HepPar1, ARG-1, CAM 5.2, and CEA.1 Positive expression of albumin by in-situ hybridization has also been shown to be a robust marker for HCC and can be more sensitive and specific in comparison to ARG-1 and HepPar1.7
In metastatic HCC, the cytologic criteria and immunophenotype are similar to that of primary HCC, however, loss of expression of the traditional immunohistochemical stains can occur.2 Cytologic specimens have an architecture of single tumor cells, trabecular pattern, traversing capillaries, surrounding endothelium, and naked nuclei.2 Cells have cytoplasmic vacuolization, prominent nucleoli, and giant tumor cells.
The cytologic features of this case were tumor cells singly or in groups, prominent nucleoli, granular cytoplasm, traversing capillaries, and some surrounding endothelial cells. The IHC staining of the lymph node biopsy determined that the cells were positive for CAM4.2, glypican-3, and focally positive for arginase while negative for HepPar-1, NKX3.1, TTF-1, and p40. In-situ hybridization for albumin was also positive.
Differential Diagnosis:
Cholangiocarcinoma is the second most common primary hepatic tumor and occurs in the bile ducts.1 Its architecture has isolated cells, crowded sheets, and cell clusters with glandular differentiation, and cells exhibit nuclear enlargement and variation in size and shape.1 It can be differentiated from HCC because its cells are cuboidal or columnar instead of polygonal, may have abundant mucin instead of bile, and it has no endothelial cells surrounding trabeculae.
Metastatic adenocarcinoma, from the breast, prostate, or GI tract, can be difficult to distinguish from metastatic HCC.2 To confirm the correct diagnosis, a detailed clinical history and appropriate IHC stains should be utilized. Cytologic features specific to each possible primary site should be considered; for example, metastatic colon adenocarcinoma tends to have a dirty necrotic background, metastatic breast adenocarcinoma may retain its ductal or lobular morphology, and metastatic prostate adenocarcinoma tends to form micro-acinar structures.2
Metastatic tumors with oncocytic cytoplasm can be differential diagnoses of HCC. For example, Hürthle cell carcinoma of the thyroid has overlapping criteria with HCC including granular cytoplasm, round nuclei, prominent nucleoli, and transgressing vessels.2 Appropriate IHC stains should be utilized to identify the primary origin of these tumors.
Malignant granular cell tumors are rare neoplasms that primarily occur in the head and neck but can be seen in the lungs.1 They are difficult to distinguish from the common benign granular cell tumors.1 They resemble metastatic HCC in that they have single cells, granular cytoplasm, nucleoli, and naked nuclei.1,2 Unlike HCC, they tend to have spindle cell morphology and mitoses.1
References:
- Cibas E, Ducatman B. Cytology. 5th ed. Philadelphia, PA: Elsvier Saunders; 2021:432-439, 588-589.
- Yan L, Jakate S, Reddy V, Gattuso P. Metastatic hepatocellular carcinoma diagnosed by fine needle aspiration: A clinical and cytologic study. Diagn Cytopathol. 2018;46(6):495-500. doi:10.1002/dc.23920
- Carr B. Hepatocellular Carcinoma. 3rd ed. [Place of publication not identified]: Springer International Publishing Switzerland; 2016:43, 409-412, 414, 580-581.
- Natsuizaka M, Omura T, Akaike T et al. Clinical features of hepatocellular carcinoma with extrahepatic metastases. J Gastroenterol Hepatol. 2005;20(11):1781-1787. doi:10.1111/j.1440-1746.2005.03919.x
- Invenizzi F, Iavarone M, Donato M et al. Pulmonary Resection for Metastasis of Hepatocellular Carcinoma Recurring After Liver Transplant: An Italian Multicenter Experience. Front Oncol. 2020;10. doi:10.3389/fonc.2020.00381
- Brar G, Greten T, Graubard B et al. Hepatocellular Carcinoma Survival by Etiology: A SEER‐Medicare Database Analysis. Hepatol Commun. 2020;4(10):1541-1551. doi:10.1002/hep4.1564
- Shahid M, Mubeen A, Tse J et al. Branched Chain In Situ Hybridization for Albumin as a Marker of Hepatocellular Differentiation. American Journal of Surgical Pathology. 2015;39(1):25-34. doi:10.1097/pas.0000000000000343