Case Presentation
Case Presentation – September 2021
Epithelioid Sarcoma
Written by: Bobbie Weaver, student, Cleveland Clinic School of Cytotechnology, Cleveland, Ohio
Patient Age: 26-year-old female
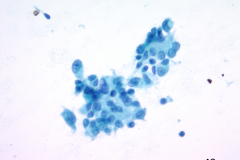
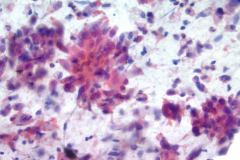
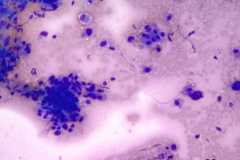
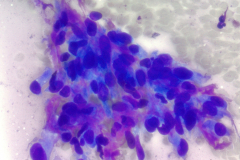
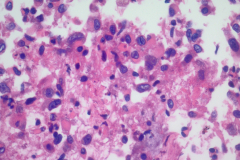
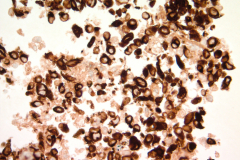
Specimen Type: FNA of RUL nodule. ThinPrep® Non-Gyn and conventional smears with Diff Quik stain, H&E stain (traditional cell block), Papanicolaou stain and AE1/AE3 (traditional cell block).
Patient History: In 2013 the patient was diagnosed with epithelioid sarcoma on the left foot. The patient had a partial foot amputation to the metacarpals. A right sentinel node biopsy was also performed which was negative. The patient has been having serial chest imaging since then. In 2017, pulmonary nodules were discovered but were very small. These nodules continued to grow slowly. In September 2019, a CT scan was performed and revealed several nodules up to 1.6 cm in size. In October 2019, an EBUS procedure was performed and an FNA of the right upper lobe nodule was taken. This FNA revealed epithelioid sarcoma. In November 2019, another CT scan was performed and a new 3mm nodule was seen. This suggests metastasis of the epithelioid sarcoma from the foot.
Cytologic Diagnosis: Epithelioid Sarcoma.
IHC: AE1/AE3, EMA and ERG – positive, CD34 – negative and loss of INI 1 expression.
Biopsy / Pathologic Diagnosis: 2013 initial diagnosis of epithelioid sarcoma on left foot. There is a current diagnosis of epithelioid sarcoma in pulmonary nodules.
Case provided by: Cleveland Clinic, Cleveland, OH
Epithelioid Sarcoma
Etiology: Epithelioid sarcoma grows along neurovascular bundles. It is a rare, slow growing soft tissue tumor. There are two types of epithelioid sarcoma. The classical type, also called distal type, is the most common. It arises in the arms or legs and can include the hands, fingers, and feet. The proximal type affects the deep soft tissue of the pelvis and perineum and is the more aggressive type.1
Clinical features: Epithelioid sarcoma affects young adults ages 15-35 years old. The lesions are usually superficial and may ulcerate causing pain for the patient. Epithelioid sarcoma recurs repeatedly and will eventually metastasize (typically to the lymph nodes) after months or years from initial diagnosis. Clinically, epithelioid sarcoma can mimic squamous cell carcinoma or granuloma.1-3
Treatment and Prognosis: Treatment usually consists of surgical excision with clean margins and with radiation before and after excision. The purpose of pre-surgery radiation is to help shrink the tumor. Post-surgery radiation helps decrease the risk of recurrence. Chemotherapy is less effective but is used in cases of metastasis. Both forms of epithelioid sarcoma have a poor prognosis. The 5-year survival rate for the classic type is 70% and drops to 35% for the proximal type.4, 5
This patient’s treatment included 21-day cycles of Gemcitabine 900mg/m2 IV on days 1 and 8, Docetaxel 75mg/m2 IV on day 8 and Pegfilgrastim on day 9. It was recommended that she protect her ovaries with Goserelin, or Leuprolide Depo starting 2 weeks prior to chemotherapy and continue for 4 weeks during chemotherapy. The patient is currently following the recommendation for treatment.
Cytology: Cytologically epithelioid sarcoma presents as numerous dispersed round, polygonal or spindle-shaped cells. Nuclei are large, vesicular, and eccentrically placed with small nucleoli. The nuclei can be single or multiple and pleomorphism may be present. The predominant arrangement is single cells, but they can also be arranged in sheets and loose cohesive clusters with fibrillary matrix. The cytoplasm is dense, may have small vacuoles with distinct cell borders. A background of necrosis is not uncommon.1-3
Differential Diagnosis:
Granuloma: Granulomas contain epithelioid histiocytes. These appear as syncytial aggregates without distinct cell borders. In necrotizing granuloma, there will be necrosis that is in the background or clinging to the histiocytes. The nuclei are elongated with pale, evenly distributed chromatin. The cytoplasm is dense and granular or vacuolated. Due to the elongated nature of the nuclei they can be confused with sarcomas or spindle cell neoplasms. Histiocytes are negative for cytokeratin and positive for CD68 and CD163.1, 3, 5
Metastatic squamous cell carcinoma: Squamous cell carcinoma can be keratinizing or non-keratinizing. The keratinizing type is easier to differentiate due to the orangeophilic cytoplasm. The non-keratinizing type has dense cytoplasm with distinct cell borders. Cells can be arranged singly, in sheets or syncytial clusters. Nuclei are central with irregular nuclear membranes. The chromatin is coarse, hyperchromatic with irregular distribution or chromatin clearing. Nucleoli are present but may or may not be prominent. In poorly differentiated squamous cell carcinoma, the cells can have a spindled appearance and may resemble sarcomas. There is also a background of necrosis. IHC for squamous cell carcinoma are CK 5/6 and p63.1-3, 5
Metastatic melanoma: Melanoma is called the great mimic because it can look like almost any neoplasm. The cells seen are usually single but can form loose bundles and can appear with a spindle cell pattern. The cytoplasm may or may not contain melanin. Cells are large, sometimes with elongated nuclei and prominent nucleoli. A typical feature to look for is intranuclear cytoplasmic inclusions. Cytoplasm contains small vacuoles or may appear dense. IHC for melanoma are S100, HMB 45, SOX 10, and MelanA.1, 3
References:
- DeMay R. The Book of Cells, A Breviary of Cytopathology. American Society for Clinical Pathology.
- Cibas ES, Ducatman BS. Cytology: Diagnostic Principles and Clinical Correlates. 4th 2014. Philadelphia, PA: Elsevier Saunders; 2014.
- DeMay R. The Art and Science of Cytopathology, Second Edition. American Society for Clinical Pathology.
- F. Brennan et al., Management of Soft Tissue Sarcoma, DOI 10.1007/978-1-4614-5004-7_14, © Springer Science+Business Media New York 2013
- Mody DR, Thrall MJ, Krishnamurthy S. Diagnostic Pathology: Cytopathology. 2nd Philadelphia, PA: Elsevier; 2018