Case Presentation
Case Presentation – June 2021
Granulosa Cell Tumor
Written by: Kathryn Iwanek, Student, Cleveland Clinic School of Cytotechnology, Cleveland, Ohio
Patient Age: 33-year-old female
Specimen Type: Cystic Mass Aspirated Fluid, ThinPrep® Non-Gyn cytology
Patient History: History of adult granulosa cell tumor (left ovary) status post resection in 2014 with new pelvic multiloculated cystic peritoneal mass concerning for recurrence.
Cytologic Diagnosis: Positive for malignant cells. Granulosa cell tumor.
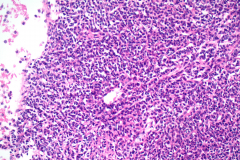
Biopsy / Pathologic Diagnosis: Soft tissue, pelvic peritoneum mass, biopsy – adult-type granulosa cell tumor.
Case provided by: Cleveland Clinic
Granulosa Cell Tumor
Etiology:
Granulosa cell tumors (GCT) are classified as sex cord-stromal tumors and account for approximately 1.5% of all ovarian tumors.1 These tumors are grouped into juvenile and adult types and the majority of cases are the adult type. GCT can occur in patients at any age, but there are peaks in occurrence for the adult type at both reproductive age and in postmenopausal women.2 Nearly all adult granulosa cell tumors involve a recurrent somatic FOXL2 mutation (p.Cys134Trp).3 Because the major function of granulosa cells include the production of sex steroids and various peptides required for folliculogenesis and ovulation, continuous exposure to ovulation induction drugs may also increase the risk of developing GCT.4
Clinical Features:
GCT are typically unilateral, slow growing tumors that are capable of metastasis.1 They occur in a younger age group and are usually detected in an early stage with many having features of hyperestrogenism.4 This increased secretion of estrogen can result in endometrial hyperplasia or carcinoma due to prolonged elevated levels of estrogen.1 Increased androgens may also be secreted and result in virilization, but that is more rare.1 The clinical symptoms of GCT are abdominal pain, abnormal vaginal bleeding, and some patients may present with menorrhagia, irregular menstruation, or amenorrhea if they are of reproductive age.2
Treatment and Prognosis:
The treatment for GCT includes surgical management in addition to chemotherapy and radiation.2 Surgery is typically the first method of treatment and although total abdominal hysterectomy and bilateral salpingo-oophorectomy is the standard, for patients who do not want to rule out the possibility of future pregnancy, unilateral salpingo-oophorectomy can be performed if the disease is confined to one ovary.2 For patients with recurrent GCT, aggressive debulking surgery should be performed.2
Patients with stage I and II GCT have a very good prognosis and do not usually require any postoperative treatment.4 Though GCT has a low malignant potential, it also has a long recurrence period. Patients require long-term follow-up since recurrence usually happens within five years after first treatment.2 The majority of recurrences are intra-peritoneal which suggests the possibility of missed peritoneal disease during primary surgery, especially for early-stage disease.4
The current patient was previously diagnosed with adult GCT and because the 8 centimeter tumor was confined to the left ovary and presented with a normal fallopian tube, underwent a left salpingo-oophorectomy in 2014. The new pelvic peritoneal mass is concerning for recurrence due to the nature of GCT and patient history.
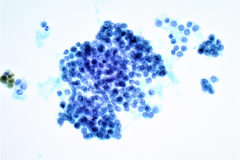
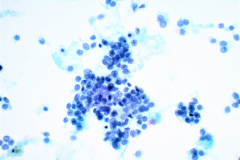
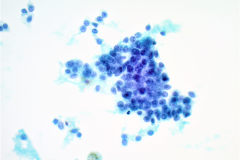
Cytology:
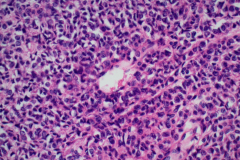
FNA samples of adult GCT are highly cellular.1 Cells typically have a centrally placed, round or oval nucleus with pale, fine chromatin and scant, poorly defined, pale cytoplasm.1 Grooved nuclei referred to as “coffee bean nuclei” are present to some degree in all cases but are not always visible on cytology.1 Characteristic Call-Exner bodies are observed in some cases as small rings of granulosa cells surrounding fluid or pyknotic nuclei.1 Naked nuclei are common and mitoses are rare.1 In some cases, nucleoli may be prominent and if Romanowsky-type stains are used, a globular basement membrane-like material may be seen as well.1
The different growth patterns of GCT include microfollicular, macrofollicular, trabecular, insular, diffuse, and moiré silk (watered silk) and can best be seen on cell block preparations.1 Despite all the different presentations however, almost one-half of cases show a prominent, arborizing vascular pattern.1
Differential Diagnosis:
Because this case is of a primary ovarian tumor presenting in a fluid, differential diagnoses for GCT as an ovarian lesion and a peritoneal mass are listed below.
Ovarian Lesion
Follicle cyst: The cytomorphology of highly cellular follicle cysts mimics that of GCT, so correlation with sonographic and laparoscopic findings is essential.5 Clinically, cellular follicle cysts are usually unilocular and completely benign.1 Cytologically, granulosa cells in a cellular follicle cyst tend to cluster haphazardly in loose spherical aggregates.1 Nuclei are round with coarsely granular chromatin and small nucleoli, though some may be pyknotic.1 In contrast to a GCT, nuclear grooves are not seen.1
Carcinoid tumor: Carcinoid tumors of the ovary are usually a component of a mature teratoma but may also present in pure form.1 Carcinoid shows numerous isolated cells, loose clusters, and occasional rosettes.1 The nuclei show characteristic “salt and pepper” chromatin and indistinct nucleoli, which contrast with the pale nuclei of the GCT.5 Carcinoid tumor cells do not have nuclear grooves as seen in GCT. Immunohistochemistry can also be used since only carcinoid will stain positive for chromogranin and synaptophysin.5
Endometrioid carcinoma: Endometrioid carcinoma of the ovary presents similarly to the usual type of adenocarcinoma of the endometrium.1 The glandular cells are numerous, elongated, palisading, and in strips of crowded or “broken” glands.1 Call-Exner bodies of GCT mimic the appearance of endometrioid tubules, but cells of endometrioid carcinoma lack nuclear grooves and often show squamous metaplasia as well.1
Peritoneal Mass
Small cell carcinoma, hypercalcemic type: Small-cell carcinoma of the ovary, hypercalcemic type is a rare and aggressive cancer which mainly occurs in adolescents and young women. Malignant cells are single or arranged in loose clusters with scant cytoplasm.6 Nuclei are hyperchromatic with smooth to irregular nuclear membranes, granular chromatin, and small nucleoli.6
Metastases: For cases in which a peritoneal mass is the first presentation or an original tumor type was not previously documented, metastatic cancers should be considered in the differentials as well. To determine the correct primary, characteristic criteria of the metastatic cancer should be observed. In the case of GCT, metastatic melanoma, breast carcinoma, or low-grade stromal sarcoma could be considered.
References:
- Cibas E. S., and Ducatman B. S. Cytology: Diagnostic Principles and Clinical Correlates: Fourth Edition. 2014. Elsevier Inc. 453-468.
- Chen YC, Chang LC, Soong RS. A late recurring and easily forgotten tumor: ovarian granulosa cell tumor. World J Surg Oncol. 2012;10:85. Published 2012 May 16. doi:10.1186/1477-7819-10-85
- Shah SP, Köbel M, Senz J, et al. Mutation of FOXL2 in granulosa-cell tumors of the ovary. N Engl J Med. 2009;360(26):2719-2729. doi:10.1056/NEJMoa0902542
- Kottarathil VD, Antony MA, Nair IR, Pavithran K. Recent advances in granulosa cell tumor ovary: a review. Indian J Surg Oncol. 2013;4(1):37-47. doi:10.1007/s13193-012-0201-z
- Atilgan AO, Tepeoglu M, Ozen O, Bilezikçi B. Peritoneal washing cytology in an adult granulosa cell tumor: A case report and review of literature. J Cytol. 2013;30(1):74-77. doi:10.4103/0970-9371.107528
- Selvaggi SM. Small-cell carcinoma of the ovary in peritoneal fluid. Diagn Cytopathol. 1994;11(3):266-270. doi:10.1002/dc.2840110314