GYN Atlas - Squamous Cell Carcinoma
SQUAMOUS CELLS
SQUAMOUS CELL CARCINOMA
R. Marshall Austin, MD, PhD
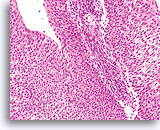
Squamous cell carcinoma (SCC) is the most common malignant neoplasm of the uterine cervix. Although sub-classification is not required by the Bethesda System, it is common to clinically subdivide these tumors into nonkeratinizing and keratinizing forms.
Before discussing the specific features of each type, general observations can be made. The cells of both keratinizing and nonkeratinizing SCC are larger than cells of carcinoma-in-situ and exhibit more definitive squamoid features. It is the cytoplasmic features that principally allow the cytologist to differentiate the lesions into nonkeratinizing and keratinizing types, while the nuclear morphology supports the diagnosis of malignancy. The conventional Pap smear sometimes exhibits air drying and smearing artifact that can distort these cancer cells and hinder a confident diagnosis as well as present abundant blood that will precipitate the air-dry artifact and obscure the cells. The ThinPrep Pap Test process allows these pleomorphic changes to be exhibited without further artifactual distortion and also lyses some blood to help prevent obscuring conditions.
The criteria for squamous cell carcinoma on the ThinPrep Pap Test are as follows:
| NON-KERATINIZING SQUAMOUS CARCINOMA | KERATINIZING SQUAMOUS CARCINOMA | SMALL CELL SQUAMOUS CELL CARCINOMA | |
| Cell Type | Non-keratinizing squamous cells | Keratinizing and few non-keratinizing squamous cells | Undifferentiated squamous cells |
| Tissue Presentation | Predominantly syncytia, scattered single cells d | Predominantly single cells with few groups | Single cells, groups and syncytia |
| Cytoplasmic Presentation | Vacuolated, cyanophilic | Dense, keratinized | Delicate, scant, basophilic |
| Nuclear Membrane | Prominent membrane irregularities | Membrane irregularities | Smooth to slightly irregular nuclear membranes |
| Chromatin | Coarse and unevenly distributed, with distinct parachromatin clearing | Pyknotic, hyperchromatic, pleomorphic | Coarse and generally evenly distributed, hyperchromatic |
| Nucleoli | Prominent macronucleoli | Occasional macronucleoli | +/- conspicuous nucleoli |
| Tumor Diathesis/Necrosis | +/- | +/- | +/- |
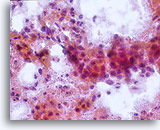
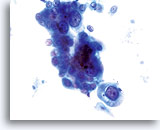
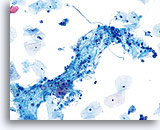
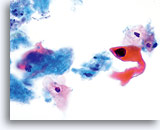
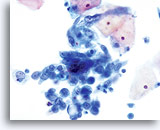
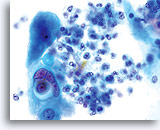
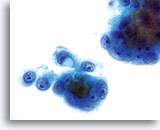
NON-KERATINIZING SQUAMOUS CELL CARCINOMA:
This is the most common form of carcinoma in the cervix. These cells tend to be medium to large in size and present predominantly in groupings or syncytial arrangements. The cytoplasm of nonkeratinizing SCC generally stains cyanophylic and will appear dense and slightly vacuolated. This vacuolization of the cytoplasm may cause the cytologist to consider a diagnosis involving a glandular lesion but the cellular criteria should re-direct you to a squamous category. The groups of non-keratinizing SCC present in a “flatter” sheet with less distinct cytoplasmic borders to the grouping than adenocarcinoma and lack the true glandular features such as rosette/acini formations, scallop borders, columnar differentiation or elongation and crowding of the nuclei.
The nuclei are enlarged with a nuclear to cytoplasmic ratio closer to that of moderate dysplasia than CIS. The classic malignant nuclear features distinguish this as a carcinoma, rather than a squamous intraepithelial lesion. The chromatin pattern is quite variable, presenting most often as coarsely granular and irregularly distributed with prominent parachromatin clearing. The nuclear envelope is highly irregular, and large irregularly shaped nucleoli are common. These features establish the diagnosis of malignancy for this entity.
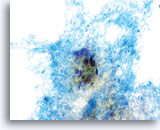
Tumor diathesis is an important characteristic of invasive carcinoma. Overall, between 50% and 80% of invasive carcinomas will manifest a diathesis on conventional Pap smears. The frequency of diathesis is similar in samples collected by the ThinPrep® method; however the typical smearing pattern of tumor diathesis/necrosis seen on the conventional Pap smear is altered. With the ThinPrep Pap Test the diathesis tends to clump upon itself, being comprised of “ratty” debris including blood, fibrin and protein strands, tissue necrosis and cellular debris, and presenting with a frayed appearance around the edges. The material can also be observed sticking to epithelial groupings.
The key look-alike entities for tumor diathesis on the ThinPrep® Pap Test are cytolysis, infection and atrophy. All of these conditions present a dirty or “ratty” looking background and when screened in context with the epithelial material present will help you determine the cause of the background. As with any situation, the cytologist should not base their diagnosis on one criterion alone. If a ratty background is the only feature present, even if it is truly diathesis, a definitive diagnosis should not be rendered. It is the morphologic features of malignancy in the epithelial cell nucleus that hold the key to the definitive diagnosis.
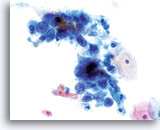
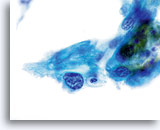
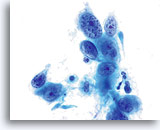
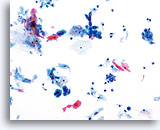
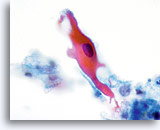
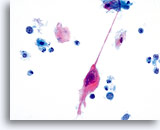
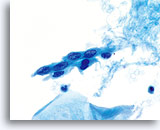
Keratinizing SCC, unlike the nonkeratinizing counterpart presents with pleomorphic, highly keratinized squamous cells. These cells vary greatly in size and shape and tend to occur singly with few small groups or syncytial arrangements.
Squamous cells with bizarre shapes; spindle, caudate tadpole, etc., present a characteristic picture on the ThinPrep® Pap Test.
The changes can be confidently identified as true pleomorphism and not due to smearing artifact. The exaggerated cell to cell variability both in cell size and more importantly, cell shape, distinguishes keratinizing SCC from keratinizing dysplastic lesions. Similar variability in the size and shape of the nuclei are also seen.
Nuclei exhibit prominent hyperchromasia, so called “ink black”, and at times can appear “ghost like” because of the abundant keratinization. Another feature observed due to the abundant keratinization is keratinized blebs of cytoplasm extending from the body of the cell. This feature lends to the pleomorphic appearance and helps to differentiate from atypical parakeratosis and keratinizing LSIL.
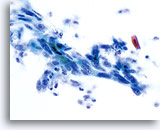
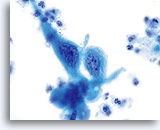
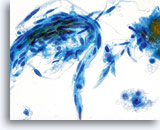
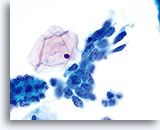
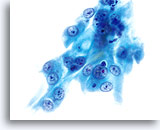
SMALL CELL SQUAMOUS CELL CARCINOMA:
Small cell (squamous cell) carcinoma can be identified using the ThinPrep® Pap Test. These lesions are composed of small, poorly differentiated epithelial cells that on first look may appear relatively uniform. An important feature highlighting the abnormality of these cells is the very high N/C ratio. They exhibit scant, fragile appearing cytoplasm and may even present as “stripped nuclei” singly and in clusters. The syncytial groupings may mimic glandular clusters but lack the roundness and 3-dimensional presentation classic to adenocarcinoma.
The nuclei are small and vary slightly in size with the nuclear membrane being fairly smooth. The chromatin pattern is often coarsely granular but tends to be evenly distributed and hyperchromatic. Because of the rapid fixation technique utilized with the ThinPrep Pap Test, nucleoli can be seen.
LOOK-ALIKE ENTITES/DIFFERENTIAL DIAGNOSES:
Keratinizing squamous cell carcinoma poses less of a diagnostic problem than non-keratinizing SCC. High grade keratinizing dysplasia may mimic carcinoma on the ThinPrep Pap Test, as with conventional Pap smears. Cautious interpretation regarding this differential is advised. Therefore, in describing look-alike entities, we will deal with the non-keratinizing entity that at times proves a much more challenging diagnosis and can have multiple differential diagnoses.
| Non-keratinizing SCC | Repair | Adenocarcinoma | |
| Presentation | Syncytial sheets with depth of focus to center of group and flat cells around the edge, groups and few single cells | Flat sheets | 3-dimensional clusters, single cells |
| Cell Type | Squamous cells | Endocervical/ metaplastic cells | Glandular cells |
| Cytoplasm | Dense, sometimes vacuolated
Irregular, angulated cytoplasmic borders Flat around edges of group with slight depth of focus at center |
Thin, vacuolated
Tissue culture appearance Flat, pulled out |
Discrete vacuoles
Distinct, prominent cell borders to the clusters Rounded-up |
| Nucleus | Irregular, sharp angles | Uniform, smooth membranes | Irregular, undulating membranes |
| Chromatin | Clumped, unevenly distributed, parachromatin clearing | Uniform, hypochromatic | Fine to coarsely granular, evenly distributed, hypo- to hyperchromatic (stealth gray appearance) |
| Nucleoli | Occasional, macronucleoli
Irregular, single or multiple |
Prominent and present in almost every cell
Small, uniform, sometimes multiple |
Prominent macronucleoli
Large, round |
There will be situations when, because of the poor differentiation of a lesion, the epithelial type cannot be specified. This situation is the same for conventional Pap smears as well as the ThinPrep® Pap Test. However, if you adhere to the recommended criteria as stated above, you will be better able to decide on the correct diagnosis.
SUGGESTED READINGS:
- Guidos, BJ et al: Use of the ThinPrep Pap Test in clinical practice. Diagnostic Cytopathology 1999;20:70-73 (Supplement to Ob.Gyn. News)
- Clark, S et al: Invasive Squamous Cell Carcinoma in ThinPrep Specimens: Diagnostic Clues in the Cellular Pattern. Acta Cytologica 2000; 44:861 (Poster Presentation)
- Inhorn, SL et al: Validation of the ThinPrep Papanicolaou Test for Cervical Cancer Diagnosis. J. of Lower Genital Tract 1998; 2:208-212
- Hutchinson, ML, et al: Evaluation of Conventional versus ThinPrep Cervical Smears in a Population-Based Study of 10,000 Women in Costa Rica. Acta Cytologica 1995; 39:969