Cytology of Pleural, Pericardial and Peritoneal Cavity Effusions - Effusions - Hematologic Malignancies
EFFUSIONS – HEMATOLOGIC MALIGNANCIES
Reminder: You may click on any slide image
for an enlarged view.
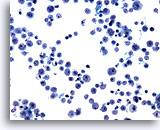
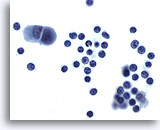
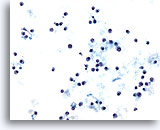
Pleural effusion:
Non-Hodgkin’s lymphoma.
20X
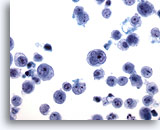
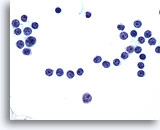
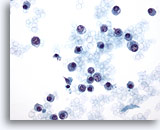
Pleural effusion:
Non-Hodgkin’s lymphoma.
40X
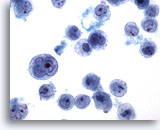
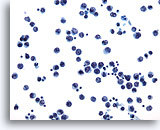
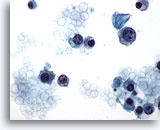
Pleural effusion:
Non-Hodgkin’s lymphoma.
60X
Figures 29-31:
By nature these cells are most often single or in small loosely adherent clusters. Non-Hodgkin’s lymphoma cells are present as a distinct population of cells which must be distinguished from mesothelial cells and from inflammatory cells or blood born leukocytes. In this set of three photomicrographs, the neoplastic population consists of lymphoid blasts, of variable size, with prominent nucleoli and irregular nuclear membrane clefts. The cells vary markedly in size but show similar cytologic characteristics.
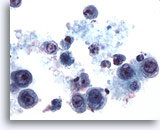
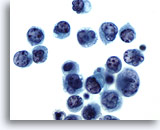
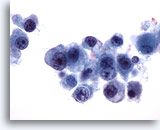
Pleural effusion:
Non-Hodgkin’s lymphoma.
60X
This pleural effusion also has a distinct population of discohesive mononuclear cells, allowing the diagnosis of lymphoma. Note the necrotic background.
Pleural effusion:
Chronic lymphocytic leukemia.
60X
The presence of small uniform lymphocytes in a pleural effusion may indicate tuberculosis, thoracic duct obstruction or leukemia/lymphoma. Chronic lymphocytic leukemia and well-differentiated lymphocytic lymphomas may include a pleural effusion consisting of small, round lymphocyte. When a question exists, flow cytometry can confirm the clonal nature of these cells.
Pleural effusion:
Chronic lymphocytic leukemia.
60X
An example of small, round lymphocytes in a pleural effusion. The differential diagnosis includes inflammatory conditions such as tuberculosis, and autoimmune diseases.
Pleural effusion:
Non-Hodgkin’s lymphoma.
20X
Pleural effusion:
Non-Hodgkin’s lymphoma.
60X
Figures 35-36:
The neoplastic lymphocytes in these two photos may appear small and monotonous, but compared to the background lymphocytes, they are considerably larger. Nuclei are vesicular, with nuclear clefting and lobation and variably prominent nucleoli.
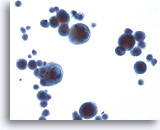
Pleural effusion:
Multiple myeloma.
20X
Pleural effusion:
Multiple myeloma.
40X
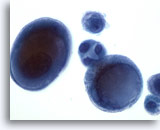
Pleural effusion:
Multiple myeloma.
60X
Pleural effusion:
Multiple myeloma.
60X
Figures 37-40:
Cells of plasmacytoma or multiple myeloma superficially resemble lymphocytes, but exhibit eccentric nuclei. The open chromatin pattern with variable nucleoli are features of plasmablasts. Again, if there is a doubt, flow cytometry can establish monoclonality.
Pleural effusion:
Malignant melanoma.
20X
Malignant melanoma cells may present in effusions with or without an antecedent skin tumor. They often metastasize to unusual places such as small bowel serosa.
Pleural effusion:
Malignant melanoma.
60X
Cells are discohesive because these are not true epithelial cells. Nuclei are large and vesicular and may include a pseudo-inclusion, which is in reality cytoplasm indenting the nuclear membrane. Pigmentation of the cytoplasm is often but not always present. Immunohistochemistry can confirm the identity of these cells either on ThinPrep slides or cell block material.